Member-only story
EBV+ Lymphoproliferative Disorder, Polymorphous Type with Hodgkin-Like Features and Extensive Necrosis
Lessons From the Friday Unknowns
The patient has a history of plasma cell neoplasm (status post SCT ), renal transplant, therapy-related MDS (status post SCT). PET-CT scan showed a cluster of prominent FDG-avid lymph nodes in the right upper neck, a conspicuously active right hilar lymph node and several ill-defined active nodules/nodes in the abdomen/upper pelvis.

Histologic sections show lymphohistiocytic infiltrate with marked necrosis.
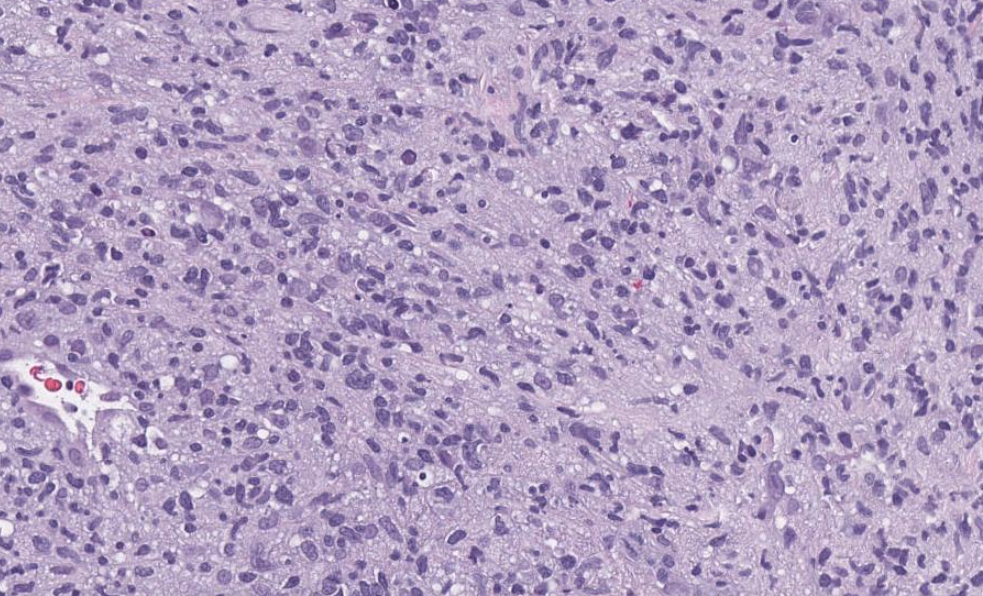

Scattered large lymphoma cells with vesicular chromatin and prominent nucleoli are identified. Some are mononucleated and some are binucleated, consistent with Hodgkin/Reed-Sternberg cells. Rare mummified cells are also present.
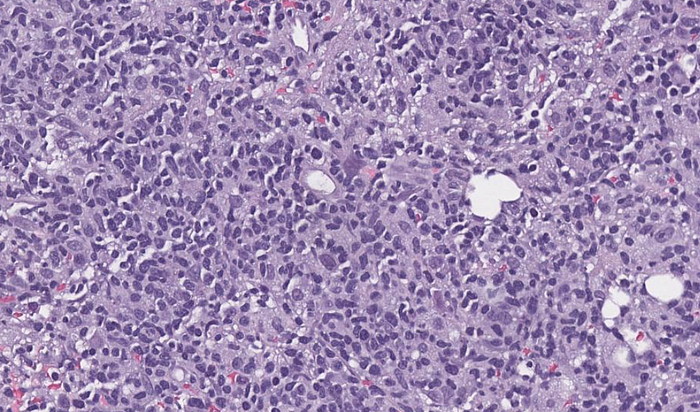

The large lymphoma cells are positive for CD30 (weak, variable), PAX5 (weak), MUM1, BOB1 (weak), OCT2, CD79a (variable), and negative for CD20, CD15, CD45, CD3, CD5, ALK, cytokeratin. CD3 and CD5 highlight many T cells in the background. CD138 highlights scattered plasma cells which appear to express polytypic kappa and lambda light chains. The proliferation index by Ki67 is ~60% in the lymphohistiocytic infiltrate. CMV and HSV stains are negative. Some of the necrotic cells appear to be CD20+ with a subset being large in size.
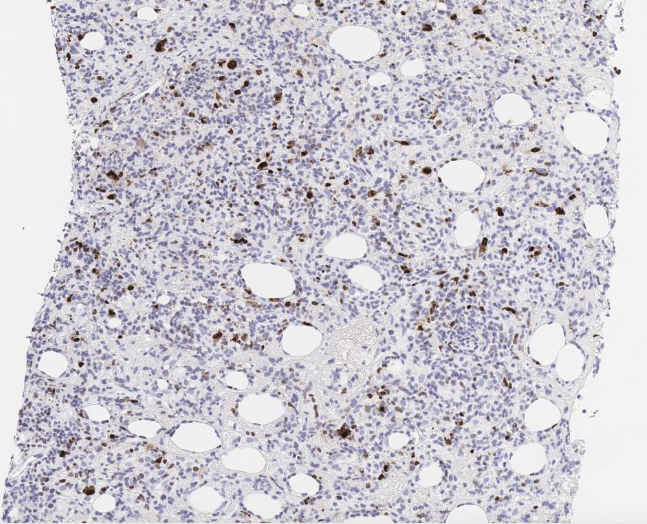
EBER by in situ hybridization is positive in scattered (small and large) cells (~10% of viable cells).